Ulcerative Colitis Diet based Case Study: Role of Fecal Calprotectin & Endoscopic Assessment in diagnosis

A 34-year-old male patient presents with a 6-month history of chronic diarrhea, passing 5–7 stools per day containing blood and mucus, accompanied by lower abdominal pain, urgency, and tenesmus. He also reports fatigue, reduced appetite, and an unintentional weight loss of approximately 4 kg.
There is no history of recent travel, antibiotic use, or acute gastrointestinal infection. Family history is significant for inflammatory bowel disease in a first-degree relative.

- Hemoglobin: 8 g/dL (mild anemia)
- Mean corpuscular volume (MCV): 72 fL (microcytic)
- Serum ferritin: low, consistent with iron deficiency

- C-reactive protein (CRP): 28 mg/L (normal <5 mg/L)
Infectious causes are excluded:
- Stool culture: Negative
- Ova and parasites: Not detected
To evaluate intestinal inflammation, fecal calprotectin is measured and found to be:
- Fecal calprotectin: 620 µg/g stool
- (Normal: <50 µg/g;
Mild elevation: 50–200 µg/g;
Active inflammatory bowel disease: >250 µg/g)
- (Normal: <50 µg/g;
These findings strongly support an active inflammatory bowel disease rather than a functional disorder such as irritable bowel syndrome.

- Diffuse erythema and edema of the rectal and sigmoid mucosa
- Loss of normal vascular pattern
- Friability with contact bleeding
- Superficial ulcerations
To determine the extent and severity of disease, a full colonoscopy is subsequently conducted. Colonoscopy reveals:
- Continuous inflammation extending from the rectum to the sigmoid colon
- No skip lesions
- Normal appearance of the proximal colon
- Normal terminal ileum
Multiple biopsies obtained during colonoscopy show:
- Crypt architectural distortion
- Crypt abscess formation
- Chronic inflammatory infiltrates in the lamina propria
These histopathological findings confirm the diagnosis of left-sided ulcerative colitis (mild to moderate activity).

- The nature of ulcerative colitis (whether it is infectious, autoimmune, or lifelong)
- The meaning and importance of fecal calprotectin
- The difference between sigmoidoscopy and colonoscopy, and why both were required
- The role of diet in triggering flares and maintaining remission
- Which foods to avoid during active disease
- Which foods may be safe or beneficial during remission
 Counselling By Pharmacist
Counselling By Pharmacist :
:
- What is the nature of ulcerative colitis (whether it is infectious, autoimmune, or lifelong)?
Ulcerative colitis is an auto-immune mediated inflammatory disease of intestine especially involving the colon and rectum with alternating stages of exacerbation and remission (decrease/disappearance). Ulcerative colitis belongs to the group of diseases known as inflammatory bowel diseases (IBD).
In ulcerative colitis, the body’s own immune system mistakenly attack the lining cells of colon and rectum causing the inflammation that isn’t curable but can be manage by anti-inflammatory, immunosuppressants and biological drugs. It may be caused by genetic disorders.
- What is the meaning and importance of fecal calprotectin?
Calprotectin test is used to measure the level of calprotectin in the stool in order to obtain the information regarding inflammation in the intestine. Under the normal condition, small amount of the calprotectin is present in the stool. However, during inflammation the level of calprotectin increases above the normal limit this is due to the involvement of the white blood cells (especially neutrophils) at the inflamed site of the intestine which releases the calprotectin in the intestinal lumen. This calprotectin then gets mixed with the stool present in the intestines.
- This test helps differentiate the Inflammatory bowel disease (IBD) from irritable bowel syndrome (IBS) as the level of calprotectin doesn’t get raised during IBS.
Some of the medicines that can interact with this test includes:
NSAIDS (Patients are usually advised to stop NSAIDs 2–4 weeks before testing, if clinically possible. This is because that NSAIDs can cause intestinal mucosal inflammation and neutrophil infiltration, leading to falsely elevated fecal calprotectin levels).
PPIs (proton pump inhibitors): Proton pump inhibitors may cause mild elevations of fecal calprotectin by following ways:
- PPIs reduce gastric acid which causes increased survival of bacteria Leading to small intestinal bacterial overgrowth and inflammation
- Chronic acid suppression may impair mucosal defense consequently leading to mild inflammation, potentially causing false-positive results.
Though other markers like C-reactive protein (CRP) and ESR (erythrocyte sedimentation rate) are often recommended on initial bases in a blood test to find out the inflammation in the body, but a calprotectin stool test is more precise at finding inflammation in the intestines.
The level of Calprotectin also gets raised during other conditions like food poisoning, intestinal or colorectal cancer, celiac disease, certain bacterial infection e.g. caused by Clostridium difficle, and due to taking NSAIDs. So, in order to confirm IBD, calprotectin test is often followed by Sigmoidoscopy or Colonoscopy (which involves the use of a minute camera to look inside your intestines).
The calprotectin level in the patient is high which suggests the possibility of IBD, confirmed later by colonoscopy
- Fecal calprotectin: 620 µg/g stool
Normal: <50 µg/g
Mild elevation: 50–200 µg/g;
Active inflammatory bowel disease: >250 µg/g
- What is the difference between sigmoidoscopy and colonoscopy, and why both were required?
Colonoscopy & flexible sigmoidoscopy are procedures that allows the doctors to look inside the rectum and the colon (large intestine) of the patient using scopes (consisting of light and a minute camera attached to a long thin tube).
Colonoscopy involves the examination of entire colon and rectum. While Flexible sigmoidoscopy involves the examination of rectum and the lower colon (sigmoid colon) only. The sigmoid colon makes about 1/3rd of the total colon.
If polyps or growths are observed during sigmoidoscopy than colonoscopy is often recommended to know about the condition of the entire colon and to take biopsies. That’s why colonoscopy following the sigmoidoscopy was recommended to the patient.
FAQ: What is the difference between flexible and rigid sigmoidoscopy?
The difference lies in the structure of scope used in the procedure and the resulting area of the intestine observed during the procedure. The rigid sigmoidoscopy involves the usage of a 25 cm long rigid tube that doesn’t bent along the intestine. It’s also called a proctoscopy (Procto means rectum). Though it can go to the sigmoid colon but is mostly used for the examination of the rectum and anus related disorders.
While the flexible sigmoidoscopy involves the usage of flexible scope that can reach even to the descending colon and is mostly used for the investigation of rectum and sigmoid colon related disorders like rectal bleeding/blood in stool, changes to pooping habits, lower abdominal or pelvic pain, haemorrhoids, inflammation, polyps, tumors or for unintentional weigh loss.
- What is the role of diet in triggering flares and maintaining remission?
Diet of the patient doesn’t cause the ulcerative colitis however some of food can aggravate the symptoms during the active state of Ulcerative colitis. Likewise, some of the foods are very good at maintaining the remission of the disease. So, the selection of the food is very important in the case of ulcerative colitis.
Basically, the nature of the food and its components can affect the bowel movement (especially considered during diarrhoea or constipation) and also the inflamed area of the colon triggering the symptoms of ulcerative colitis.
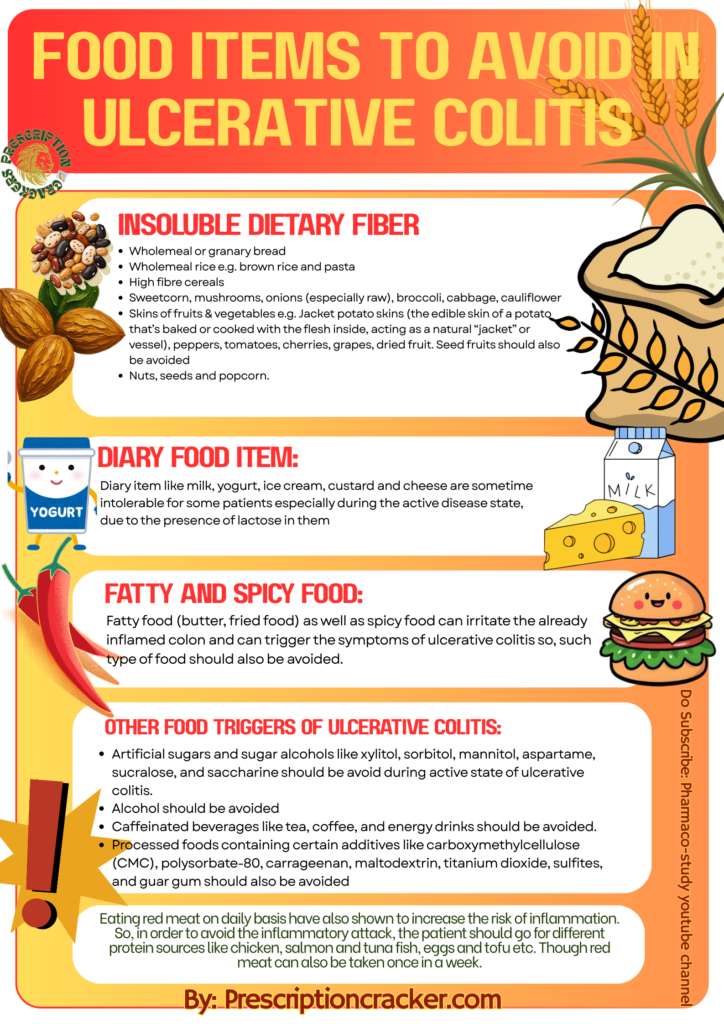
- Which foods to avoid during active disease?
Dietary fibres are of two types: soluble dietary fibre and insoluble dietary fibre (does not dissolve in water). Insoluble dietary fibre should be avoided during the active disease as they can irritate the already inflamed area of the colon and can also speed up the bowel movements that can aggravate the diarrhoeal condition. While soluble dietary fibre can be taken during active disease and for the maintenance of the remission
Following is the list of insoluble dietary fibres that should be avoided during the active disease state.
- Wholemeal or granary bread
- Wholemeal rice e.g. brown rice and pasta
- High fibre cereals
- Sweetcorn, mushrooms, onions (especially raw), broccoli, cabbage, cauliflower
- Skins of fruits & vegetables e.g. Jacket potato skins (the edible skin of a potato that’s baked or cooked with the flesh inside, acting as a natural “jacket” or vessel), peppers, tomatoes, cherries, grapes, dried fruit. Seed fruits should also be avoided
- Nuts, seeds and popcorn.
Diary food item:
Diary item like milk, yogurt, ice cream, custard and cheese are sometime intolerable for some patients especially during the active disease state, due to the presence of lactose in them. Avoiding these dairy items means avoiding major sources of calcium which can create bone health disorders. Thus, it is often recommended, to lactose intolerant patients, to include following food items in their diet as an alternative source of calcium:
- Low Lactose or Lactose Free milks and milk products.
- Rice, soya, or Oat milks fortified with calcium.
- Hard cheese instead of soft cheese may be tolerated better.
Fatty and Spicy food:
Fatty food (butter, fried food) as well as spicy food can irritate the already inflamed colon and can trigger the symptoms of ulcerative colitis so, such type of food should also be avoided.
Other food triggers of ulcerative colitis:
- Artificial sugars and sugar alcohols like xylitol, sorbitol, mannitol, aspartame, sucralose, and saccharine should be avoid during active state of ulcerative colitis.
- Alcohol should be avoided
- Caffeinated beverages like tea, coffee, and energy drinks should be avoided.
- Processed foods containing certain additives like carboxymethylcellulose (CMC), polysorbate-80, carrageenan, maltodextrin, titanium dioxide, sulfites, and guar gum should also be avoided
Eating red meat on daily basis have also shown to increase the risk of inflammation. So, in order to avoid the inflammatory attack, the patient should go for different protein sources like chicken, salmon and tuna fish, eggs and tofu etc. Though red meat can also be taken once in a week.
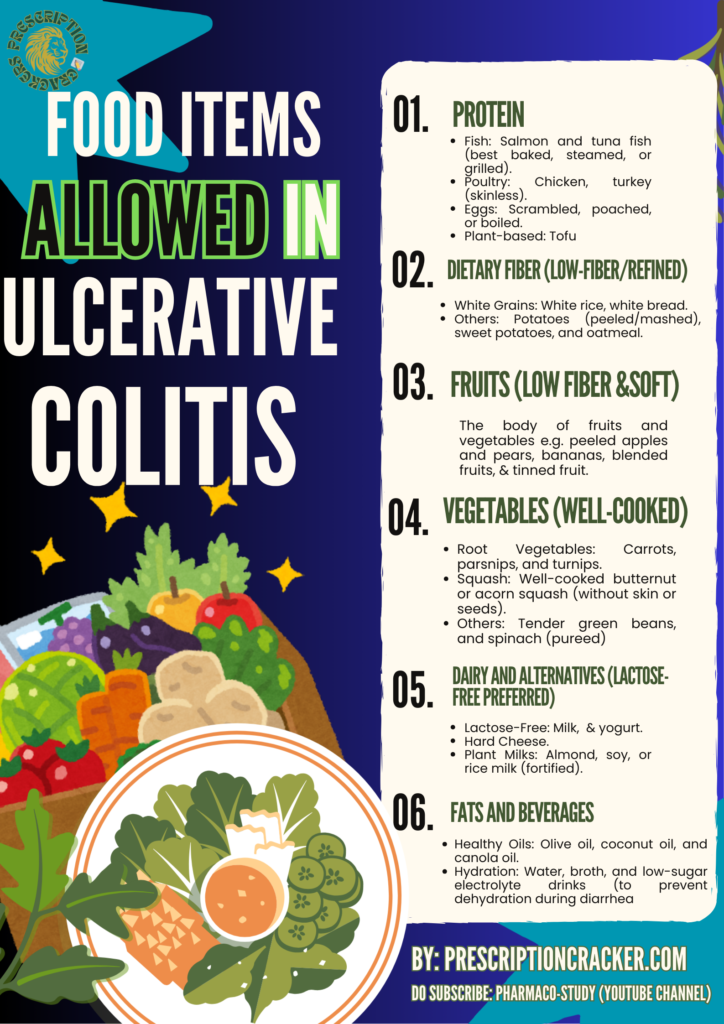
- Which foods may be safe or beneficial during remission?
Food items that are safe and beneficial during remission phase of ulcerative colitis are mentioned in the image below:
References:
Radziszewska, M., Smarkusz-Zarzecka, J., Ostrowska, L., & Pogodziński, D. (2022). Nutrition and supplementation in ulcerative colitis. Nutrients, 14(12), 2469. https://doi.org/10.3390/nu14122469
MedlinePlus. (n.d.). Calprotectin stool test. U.S. National Library of Medicine. https://medlineplus.gov/lab-tests/calprotectin-stool-test/
MedlinePlus. (n.d.). Colonoscopy. U.S. National Library of Medicine. https://medlineplus.gov/colonoscopy.html
Cleveland Clinic. (n.d.). Flexible sigmoidoscopy: What it is, purpose, prep, vs colonoscopy. https://my.clevelandclinic.org/health/diagnostics/4953-flexible-sigmoidoscopy
Johns Hopkins Medicine. (n.d.). Sigmoidoscopy. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/sigmoidoscopy
Milton Keynes University Hospital NHS Foundation Trust. (n.d.). Dietary advice for ulcerative colitis. https://www.mkuh.nhs.uk/patient-information-leaflet/dietary-advice-for-ulcerative-colitis-2
Crohn’s & Colitis Foundation. (n.d.). What should I eat with Crohn’s or colitis? IBD diet guide. https://www.crohnscolitisfoundation.org/patientsandcaregivers/diet-and-nutrition/what-should-i-eat