Menstrual Migraine Case Study-Cyclical Headache in a Young Woman with Fatigue and Menorrhagia

 Patient Profile
Patient Profile
A 29-year-old female school teacher presents to a neurology outpatient clinic with a 7-year history of recurrent headaches that have worsened over the last 12 months. She reports that the headaches occur predictably every month, beginning one to two days before the onset of menstruation and lasting up to three days. As per doctors, she is having menstrual migraine.
She describes the pain as unilateral, throbbing, predominantly over the right temporal region, with moderate to severe intensity. The headache is accompanied by nausea, photophobia, phonophobia, and marked fatigue, forcing her to miss work at least one day per cycle. She denies aura but reports increased irritability and food cravings prior to headache onset.
The patient reports regular menstrual cycles (28–30 days) but complains of heavy menstrual bleeding for the past 3–4 years, requiring frequent pad changes during the first two days of menstruation. She denies intermenstrual bleeding. No history of hormonal contraceptive use is reported. There is no history of pregnancy.
 Associated Symptoms
Associated Symptoms
Over the last year, the patient has noticed:
- Progressive generalized weakness
- Shortness of breath on exertion
- Difficulty concentrating during migraine episodes
- Increased craving for ice and chalk (reported casually)
- Muscle tightness and occasional calf cramps during menstruation
She also reports that headaches are worse during periods of stress, poor sleep, and when she skips meals during workdays.
 Past Medical and Drug History
Past Medical and Drug History
- No history of hypertension, diabetes, or thyroid disease
- Uses OTC NSAIDs intermittently for headache relief with partial benefit
- Drinks 2–3 cups of tea daily
- No history of smoking or alcohol use
- No known drug allergies
Family history reveals migraine in her mother and iron deficiency anemia in her elder sister.

- Pale conjunctiva noted
- BMI: 21.8 kg/m²
- Blood pressure: 104/66 mmHg
- Pulse: 88/min, regular
- Neurological examination: normal
- No focal neurological deficits
 Laboratory Investigations
Laboratory Investigations
|
Test |
Patient Value |
Reference Range |
|
Haemoglobin (Hb) |
9.6 g/dL |
12.0–15.5 g/dL |
|
Mean Corpuscular Volume (MCV) |
72 fL |
80–96 fL |
|
Mean Corpuscular Hemoglobin (MCH) |
22 pg |
27–33 pg |
|
Serum Ferritin |
8 ng/mL |
15–150 ng/mL |
|
Serum Iron |
38 µg/dL |
50–170 µg/dL |
|
Total Iron Binding Capacity (TIBC) |
460 µg/dL |
250–370 µg/dL |
|
Transferrin Saturation |
8% |
20–50% |
|
Serum Magnesium |
1.5 mg/dL |
1.7–2.4 mg/dL |
|
Vitamin D (25-OH) |
18 ng/mL |
30–100 ng/mL |
|
Vitamin B12 |
420 pg/mL |
200–900 pg/mL |
|
TSH |
2.1 mIU/L |
0.4–4.0 mIU/L |
 Clinical Pattern Observed
Clinical Pattern Observed
The patient maintains a headache diary, which reveals:
- Headache onset consistently between day −2 and day +1 of menstruation
- No headaches during mid-cycle or ovulation
- Increased severity during cycles with heavier bleeding
- Reduced response to usual analgesics during menstruation compared to other headaches
 Psychosocial Context
Psychosocial Context
The patient reports high occupational stress, irregular meal timing, and poor sleep during examination periods at school. She expresses concern about long-term medication use and prefers “natural options” if possible but is open to medical treatment if clearly explained.
Counselling & Discussion Prompts (For Learners / Clinicians)
This case requires discussion and counselling regarding:
- Identification of menstrual migraine triggers beyond hormonal changes.
- The possible role of haematological abnormalities in headache frequency and severity.
- Selection of acute and preventive allopathic therapies specific to menstrual patterns
- Role of nutritional and micronutrient supplementation
- Lifestyle counselling including diet, caffeine use, sleep hygiene, and stress management.
- Patient education on headache diaries and trigger avoidance
 Pharmacist’s Workup for menstrual migraine case study:
Pharmacist’s Workup for menstrual migraine case study:
- Identification of menstrual migraine triggers beyond hormonal changes.
Migraine is an intricate neurovascular inherited disorder characterized by the over excitation of neurons and the activation of trigeminovascular system, resulting in the secretion of neuropeptides like cGRP, vasoactive peptide, Substance P and neurokinin A. These neuropeptides induce vasodilation, plasma protein extravasation, and sterile neurogenic inflammation (i.e. without infection, caused by any chemical, physical, metabolic or any other harmful stimuli) around blood vessels of meninges.
When talking about menstrual migraine, the scenario becomes more multifaceted. Menstrual migraines are usually associated with a sudden drop in estrogen levels just before menstruation.
However, not all women with migraine are sensitive to estrogen fluctuation, probably due to variation in estrogen receptor sensitivity or genetic factors. It has been found that menstrual migraine differs from other migraines types in several biological ways, including changes in magnesium levels, platelet behavior, nitric oxide production, prostaglandins, prolactin, opioid pathways, and dopamine function
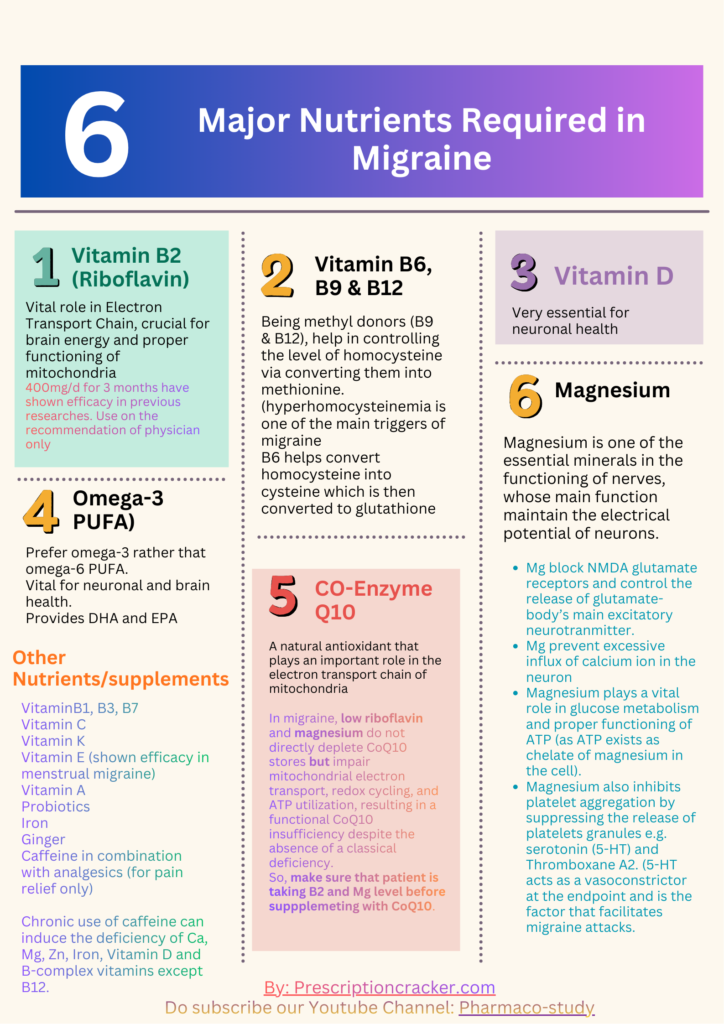
Nutritional triggers of Menstrual Migraine:
- Iron deficiency Anemia- Iron plays an important role in the synthesis and metabolism of serotonin, dopamine, and norepinephrine.
- Magnesium Deficiency- (For Role of Magnesium in migraine: Read Case Study-2)
- Vitamin E deficiency (less common)- Vitamin E has positive effects on migraines and related diseases through its antioxidant function.

- Other nutritional deficiencies include: Vitamin B2, B6, B9 & B12, Vitamin D, omega-3 PUFA, Co-enzyme-Q10, & Zinc etc.
Though, Magnesium and iron are more studies in relation with menstrual migraine but the treatment approach should be based upon the identification of the deficient nutrients and then recompensation with those nutrients whether from diet or from supplements available in the market
Lifestyle triggers:
- Skipped meals can cause hypoglycemia (drop in blood sugar), which can induce the migraine attack.
- Sleep deprivation and stress can raise cortisol level which serves to increase migraine threshold and activation of trigeminovascular system.
- Caffeine (in form of tea) dependence is also considered as a trigger in this case, not only because of the nutrient depletion but also due to rebound headaches in case of withdrawal during busy routine.
- What is the possible role of hematological abnormalities in migraine frequency and severity, define in relation to this case.
|
Test |
Patient Value |
Reference Range |
|
Haemoglobin (Hb) |
9.6 g/dL |
12.0–15.5 g/dL |
|
Mean Corpuscular Volume (MCV) |
72 fL |
80–96 fL |
|
Mean Corpuscular Hemoglobin (MCH) |
22 pg |
27–33 pg |
|
Serum Ferritin |
8 ng/mL |
15–150 ng/mL |
|
Serum Iron |
38 µg/dL |
50–170 µg/dL |
|
Total Iron Binding Capacity (TIBC) |
460 µg/dL |
250–370 µg/dL |
|
Transferrin Saturation |
8% |
20–50% |
Hematological parameters are not the direct headache triggers, but they act as modifiers of the migraine threshold. When these parameters are abnormal, the brain becomes more vulnerable to otherwise physiological triggers (such as estrogen withdrawal in menstrual migraine).Hematological abnormalities in this case are manifested by the dysregularities of hemoglobin, MCV, MCH, serum ferritin, serum iron, and Transferrin saturation. Now let’s decode the meaning of these parameters in order to understands what deficiencies they are pointing at.
|
Test |
Patient Value |
Reference Range |
Meaning |
|
Haemoglobin (Hb) |
9.6 g/dL |
12.0–15.5 g/dL |
Anemia |
|
Mean Corpuscular Volume (MCV) |
72 fL |
80–96 fL |
Low level of MCV represents iron deficiency anemia |
|
Mean Corpuscular Hemoglobin (MCH) |
22 pg |
27–33 pg |
Low MCH level also represents iron deficiency anemia. |
|
Serum Ferritin |
8 ng/mL |
15–150 ng/mL |
Ferritin is a protein that stores iron. Low level of ferritin indicates fewer iron stores in the body representing iron deficiency in the body |
|
Serum Iron |
38 µg/dL |
50–170 µg/dL |
Indicates low serum iron level |
|
Total Iron Binding Capacity (TIBC) |
460 µg/dL |
250–370 µg/dL |
TIBC reflects the amount of transferrin, the primary iron-transporting protein, in your blood. |
|
Transferrin Saturation |
8% |
20–50% |
Transferrin is body’s iron-transport protein. Low level of transferrin saturation indicates low iron level in the body to be carried by transferrin protein. While higher level indicates excess iron/hemochromatosis or inflammation. |
Almost all the haematological parameters in this lab report, indicate the iron deficiency anaemia particularly low hemoglobin level. So, in this case recompensation of iron whether from diet or from marketed supplements is recommended.
FAQ: What if the MCV and MCH were higher than the normal level?
If the MCV and MCH were higher than the normal level they would indicate the deficiency of Vitamin B9 & B12 and the management would be different in that case.

Effect of Iron Deficiency on the Frequency and severity of Migraine:
When blood abnormalities such as anemia are present, oxygen delivery to the brain is reduced. The migraine brain is highly energy-sensitive, so even mild cerebral hypoxia can increase neuronal excitability and facilitate activation of the trigeminovascular system, leading to more frequent and more severe attacks.
Abnormal hematological parameters, especially iron deficiency anemia, can also disrupt neurotransmitter systems involved in migraine, particularly dopamine and serotonin. These neurotransmitters normally help regulate pain perception, nausea, and vascular tone. When their function is impaired, the brain’s endogenous pain-inhibitory mechanisms weaken, allowing headaches to become more intense and harder to control.
In addition, iron deficiency impairs mitochondrial energy metabolism, reducing ATP availability in neurons. Energy-depleted neurons have a lower firing threshold, which promotes cortical spreading depression and increases migraine susceptibility. This explains why headaches may worsen with longer duration of anemia or chronic migraine.
Hematological abnormalities may also affect vascular and platelet function, contributing to altered nitric oxide signaling, platelet serotonin handling, and neurogenic inflammation, all of which can amplify migraine severity.
Patients with iron-deficiency anaemia had a high frequency of migraine, especially observed in females. Men had comparatively lower demand for iron than women, and ferritin levels in the body of men had been quite stable, so the effect of ferritin on men may not be as significant as that on women.
FAQ: Does Estrogen have any impact on iron metabolism?
Yes, Estrogen also plays a vital role in the metabolism of iron. Estrogen influences hepcidin, a hormone that controls iron absorption and storage, and also regulates ferroportin, a key protein that transports iron out of cells. Estrogen inhibits hepcidin synthesis in liver cell and maintains integrity of ferroportin integrity on the surface of iron-releasing duodenal enterocytes, hepatocytes, and macrophages, which tends to increase circulating iron availability. This shows that estrogen has strong influence on the absorption, storage and release of iron in the body. Thus, changes in the estrogen level during the menstrual cycle could affect the metabolism of iron.
- Which allopathic Treatment options are available that are specific to the menstrual patterns?
A headache and menstrual diary can help the patient and the doctor in the identification of the best treatment strategy for the patient. When it comes to allopathic therapy, Women with menstrual migraine who have painful cramps may benefit more from a NSAID strategy with a triptan for rescue. Those who have foreseeable menstrual cycles and migraine attacks, may be help with mini-prevention strategy. Those who don’t have regular cycles can try other options.
It is also important to discuss with your doctor any personal risk factors you may have for taking oral contraception, such as an increased risk of stroke, heart disease or blood clots, as hormonal birth control can affect women with migraine differently. Please let your provider know if you have migraine with aura when discussing hormonal options.
There are basically three types of treatment strategies, in allopathic system of medicines for migraine, that vary in terms of the timings of initiation of the treatment. These three treatment strategies are mentioned in the chart given below:
- What is the role of nutritional and micronutrient supplementation?
Nutritional and micronutrients supplements play a significant role in the prevention of the migraines especially menstrual migraine. The key nutrients that are comparatively more significant in the terms of the role they play in mitochondrial, brain and neuronal functioning include:
- Riboflavin (Vitamin B2)
- Magnesium
- Vitamin B6, B9 & B12 (especially in case of hyperhomocysteinemia)
- Vitamin D
- Omega-3 PUFA
- Co-enzyme Q10
- Iron (Especially, In case of anemia) and other minerals like Zinc and Calcium
- Vitamin E
However, as per researches, Magnesium and Iron deficiencies are more likely to be associated with menstrual migraines. Likewise, in the case under study we can observe the iron and magnesium deficiencies along with the deficiency of Vitamin D. Thus, in this case, it’s very essential to recompense these nutrients, as a part of preventive therapy.
- What lifestyle counselling including diet, caffeine use, sleep hygiene, and stress management, would be given to this patient.
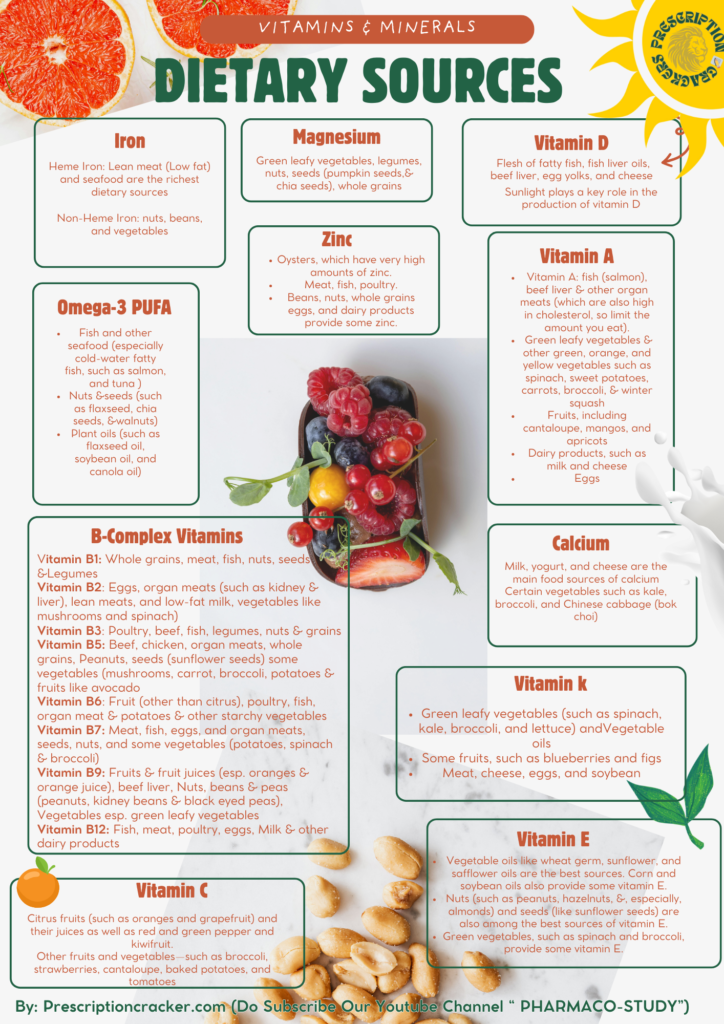
Firstly, it’s very essential to incorporate iron, magnesium and vitamin D rich foods in the diet of the patient as they are evidently deficient in this patient.
Following is the guide for the dietary sources of various vitamins and minerals which can be given to the patient for the repletion of deficient nutrients and micronutrients through the diet.
5 Cs
The patient is also informed to avoid most common triggers of migraine often known as 5 Cs migraine triggers. These includes:
- Chocolate
- Cheese
- Coffee
- Coke
- Citrus fruits.
Other reported triggers that can induce migraine attack in some people, that are sensitive to it, includes:
- Monosodium glutamate (MSG)
- Histamine
- Nitrates
- Aspartame
- Tyramine
-
Caffeine Use:
Few modifications in the diet are also required like reduction of tea intake this is because of the caffeine and tannins that are present in the tea. Tannins form complex with nutrients like iron, magnesium, zinc and other nutrients and hinder their absorption. While caffeine intake can increase excretion of magnesium, zinc, potassium, sodium and other minerals. Caffeine can hinder the absorption of iron and metabolism of Vitamin B1. Caffeine also inhibits vitamin D receptors and consequently reduces the activity of Vitamin D. Thus, in order to conserve these vitamins and minerals, caffeine and tannin intake in the form of tea should be limited to ≤1–2 cups/day.
Sleep Hygiene & Stress Management:
Sleep hygiene: For maintaining sleep hygiene, patient should be encouraged to follow following measures:
- Fixed sleep–wake time
- No screens 1 hour before bed
- Address exam-period sleep debt
Stress management: Patient undergoing stress are recommended to take following steps for the reduction of the stress:
- Short daily walks
- Breathing exercises
- Migraine-specific relaxation techniques
References
Frontiers. (2021). Nutrition. Frontiers in Nutrition. https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.685564/full
Gür-Özmen, S., & Karahan-Özcan, R. (2016). Iron deficiency anemia is associated with menstrual migraine: A case–control study. Pain Medicine, 17(3), 596–605. https://doi.org/10.1093/pm/pnv029
Wang, Y., Wang, Y., Yue, G., & Zhao, Y. (2023). Energy metabolism disturbance in migraine: From a mitochondrial point of view. Frontiers in Physiology, 14, 1133528. https://doi.org/10.3389/fphys.2023.1133528
Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of migraine: A disorder of sensory processing. Physiological Reviews, 97(2), 553–622. https://doi.org/10.1152/physrev.00034.2015
Yang, Q., Jian, J., Katz, S., Abramson, S. B., & Huang, X. (2012). 17β-Estradiol inhibits iron hormone hepcidin through an estrogen responsive element half-site. Endocrinology, 153(7), 3170–3178. https://doi.org/10.1210/en.2011-2045
American Migraine Foundation. (n.d.). Menstrual migraine: Treatment and prevention. https://americanmigrainefoundation.org/resource-library/menstrual-migraine-treatment-and-prevention/
de Mora, F., & Meßlinger, K. (2024). Is calcitonin gene-related peptide (CGRP) the missing link in food histamine-induced migraine? A review of functional gut-to-trigeminovascular system connections. Drug Discovery Today, 29(4), 103941. https://doi.org/10.1016/j.drudis.2024.103941
Research Articles & Case Studies
Disclaimer
This case study is for informational and educational purposes only. It does not substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before starting any medication